DR HARINDER SINGH BEDI
Director,
Cardio-Vascular Endovascular & Thoracic Sciences
Park Hospital, Mohali
VASCULAR disease is a major health problem in India. One in 20 people over 50 years of age have it. The total number of cases are over 42 million. More than half of those affected may not even know about the disease till it is too late. Vascular disease is not just “poor circulation.” It comes in various forms: peripheral arterial disease affects the arteries taking blood to the arms and the legs, carotid artery disease affects the arteries taking blood to the brain, and renal artery disease limits the blood flow to the kidneys causing high blood pressure or renal failure. Arterial disease is most often caused by atherosclerosis (hardening of the arteries). When atherosclerosis develops, the normally smooth linings of the arteries become narrow and rough from the buildup of plaque, which is made up of cholesterol and calcium deposits.
The severity of the blockage can be assessed by a diligent history taking a good clinical examination followed by noninvasive tests.
NONINVASIVE TESTS
A number of noninvasive tests are available to determine the presence and/or extent of vascular disease. In fact August is International Vascular Month and various camps have been organized to detect and treat patients of vascular disease.
• Ankle-Brachial Index - The most common test for PVD is the measurement of blood pressure with a special ultrasound stethoscope and machine at the ankle and its comparison with that at the elbow - the ankle-brachial index (ABI). This is a painless and fairly sensitive test which gives some idea about the severity of the disease. It also is useful in following the patient’s progress after medication or surgery. The comparison of the two numbers determines if the patient has peripheral vascular disease and if more tests are needed.
• Vascular Ultrasound - This simple, noninvasive test is very important to evaluate the arteries and veins and is the first choice for evaluation.
• Computed Tomography Angiography - A CT scan is a common radiologic test, which can be tuned to study the blood vessels (Figure 1). This test is very important for assessing aneurysms of the aorta and other vessels.
• Magnetic Resonance Angiography - Magnetic resonance imaging, commonly known as MRI, makes images of the body using a very strong magnet. The images can be focused to provide images of the arteries.
The German Epidemiological Trial on Ankle-Brachial Index (getABI) concluded that peripheral artery disease (PVD) should be treated in the same way as patients with heart disease, as PVD patients are currently undertreated. GetABI showed that PVD patients have a substantially increased risk of death-dying, on average, 10 years earlier than their peers-and that asymptomatic PVD patients are as much at risk as symptomatic ones, a vital fact that was not previously appreciated.
INVASIVE TESTS
Depending on the results of the noninvasive tests that have been performed, your surgeons may order angiograms for further evaluation of the disease.
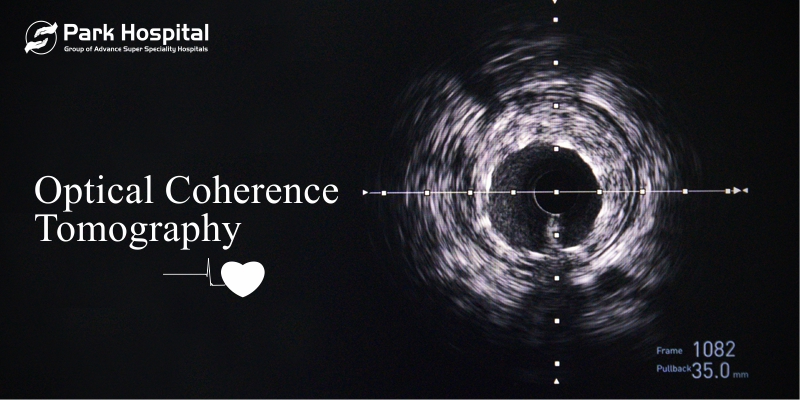
• Angiography - The most accurate test of the blood vessels is an angiogram. In this test, a small needle is put through the skin and into an artery at the top of the leg. A small plastic tube is then slid into the arterial system. X-ray contrast is then injected into the arterial system so that X-ray images of the vessels can be taken. During angiography, additional images can be obtained, using intravascular ultrasound (IVUS). A small ultrasound device is advanced into the arterial or venous system. The IVUS is useful for measuring blood vessels and for obtaining images of atherosclerotic plaque and other abnormalities.
• CT Angiography: This is a simple noninvasive test. The CT machines today are much more sophisticated and can give results as good or better than the conventional angiography with no injection into the arteries.
TREATMENT OPTIONS
Individual treatment options depend on a number of factors that will be explained by the surgeons. One size does not fit all in managing the disease. Often a combination of risk reduction, medicines, less invasive treatment options and surgery provides the patient with the best chance for a good outcome.
Risk Factor Modification / Management: For patients with mild or early stages of vascular disease, lifestyle modification and medical management of risk factors can slow down the progression of disease to the point that the individual may never need surgery or endovascular intervention.
• Lifestyle changes include
• Stopping smoking - MOST IMPORTANT
• Managing diabetes, high blood pressure and high cholesterol levels
• Regular graded exercise - including yoga
• Following a heart healthy diet.
In addition, anti-platelet medications (Aspirin or Clopidogrel), anti-hypertensive medications, blood vessel dilators and lipid-lowering medications all may be used in the medical management of vascular disease.
If the cause is an acute blood clot it may respond to medicines which dissolve the clot. This means the use of thrombolytics (clot busters) or a minor surgical procedure - embolectomy - to remove the clot. New devices are now being used to mechanically remove the clots by an endovascular route.
SURGICAL OPTIONS
Surgery is a time tested and reliable option for most vascular disorders:
Vascular bypass - This procedure uses synthetic material or a portion of a person’s own vein to route blood around a blockage in an artery. This is the most common surgical technique used in treating peripheral artery disease. The bypass material is sewn into the blood vessel above the blockage and then sewn below the blockage. This creates a new pathway for the blood to travel through. Bypass can be used to treat blockages in the legs, kidney arteries and aorta. A world first surgery documented in the Indian Heart Journal (The first ever radial artery as a conduit in femoro-popliteal bypass: a case report” Bedi HS, Mahendru PL, Suri A et al Ind Heart J 1999: 51: 310 – 312). was innovated by the author to prevent gangrene of the leg by transplanting an artery from the hand (Figure 2,3,4).
• Endarterectomy - This is a procedure in which the blood vessel is opened and plaque is removed or scraped out of the artery to restore blood flow through the vessel. The artery then is closed with a patch that makes the vessel wider. This works best for narrow areas or complete blockages of an artery. This procedure is used to treat blockages in the carotid arteries, which feed blood to the brain, and is sometimes used for other blood vessels in the upper leg.
• Aneurysmectomy - This involves placing graft material in an aneurysm so that blood flows through the graft. The aneurysm collapses against the wall of the graft, and is no longer at risk for rupture. This is used for treatment of any type of aneurysm.
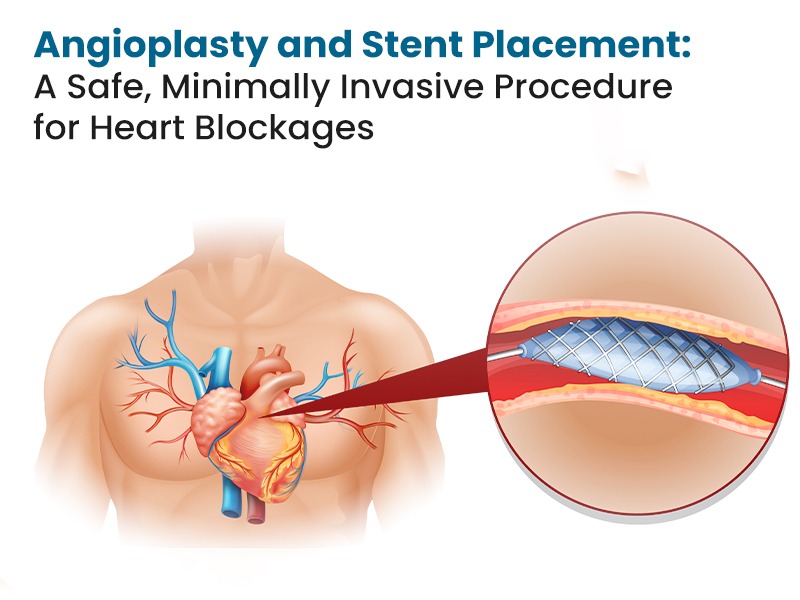
• ENDOVASCULAR SURGERY - These procedures are minimally invasive and require only a small puncture in the groin, very similar to Angiography. A balloon is inflated at the blockage and a spring (stent) is used to prop the artery open. Now vascular surgeons are getting more skilled at tackling even major disorders eg abdominal aortic aneurysms with minimally invasive or noninvasive procedures with success. The hardware for these procedures is getting more sophisticated and we ie CardioVascular surgeons are getting more skilled – hence more and more complex diseases are being successfully tackled by endovascular surgery.
PREVENTING PVD
In the early stages the use of dietary modifications - basically, a low-fat vegetarian diet, weight reduction (if overweight), graded exercise, along with the use of blood thinners, vessel dilators and cholesterol reducing drugs (statins) - help to prevent the progression of the blockage and encourages the development of collaterals.
Regular exercise is the most consistently effective treatment for PVD. Exercise programmes include simple walking regimens, leg exercises and treadmill exercises under expert supervision three or four times a week. Avoidance of smoking and all other former of tobacco use is mandatory if a permanent solution is to be got.
In diabetes the risk of narrowing of the arteries by a build-up of fat and cholesterol (atherosclerosis) is much more than in non-diabetics. The patient must inspect his feet between toes and pressure areas using a mirror regularly. He must wash his feet daily with soap and lukewarm water. He must avoid tight-fitting shoes and very hot water, hot water bottles or chemicals (to treat corns) on the feet.
Thus, simple measures should be taken from an early stage in life to prevent a crippling and even life-threatening condition from developing.
RISK FACTORS
Cigarette smoking is the No 1 risk factor for developing vascular disease
• Obesity
• Diabetes mellitus
• High cholesterol and lipids
• Heart disease
• High-stress lifestyle
• Older than age 50
• Sedentary lifestyle
• High blood pressure
SYMPTOMS
(Patients with any of these disorders may also have no symptoms):
PERIPHERAL ARTERY DISEASE:
• Leg pain with exercise known as claudication
• Leg swelling
• Weakness or tiredness in the legs
• Sores on feet or legs that won’t heal
CAROTID ARTERY DISEASE:
• Temporary loss of vision in one eye, or blurred or double vision
• Confusion
• Loss of balance or coordination
• Numbness or weakness on one side of the body
• Slurred speech or difficulty speaking
• Change in ability to use arms and legs
• Stroke
ABDOMINAL AORTIC ANEURYSM:
• Often no symptoms
• Sudden onset of abdominal or back pain
RENAL ARTERY DISEASE:
• High blood pressure (hypertension)
• Acute renal (kidney) failure
MESENTERIC ARTERY DISEASE:
• Abdominal pain, especially after eating
• Unwanted weight loss
VENOUS DISEASE:
• Leg swelling
• Sores on lower legs that do not heal
• Leg pain
DILATED VARICOSE LEG VEINS
ARE YOU AT RISK?
Take this short quiz to see if you could be at risk for peripheral vascular disease (PVD).
Q. 1 ARE YOU AGE 50 OR OLDER?
Yes No
Q. 2 DO YOU SMOKE?
Yes No
Q. 3 DO YOU HAVE DIABETES?
Yes No
Q. 4 DO YOU HAVE HIGH BLOOD PRESSURE?
Yes No
Q. 5 DO YOU HAVE HIGH CHOLESTEROL?
Yes No
Q. 6 DO YOU HAVE A FAMILY HISTORY OF HEART DISEASE OR VASCULAR (BLOOD VESSEL) DISEASE?
Yes No
Q. 7 ARE YOU OVERWEIGHT?
Yes No
Q. 8 ARE YOU SEDENTARY WITH LITTLE OR NO EXERCISE?
Yes No
If you answered yes to even one of these questions, you could be at risk for PVD.
A simple checkup by your doctor should be done.
The author is Director, Cardio-Vascular Endovascular & Thoracic Sciences at the Park Hospital, Mohali. He was previously at the Escorts Heart Institute, New Delhi and the St Vincents Hospital in Sydney. He is a Senior member of the prestigious IACTS.